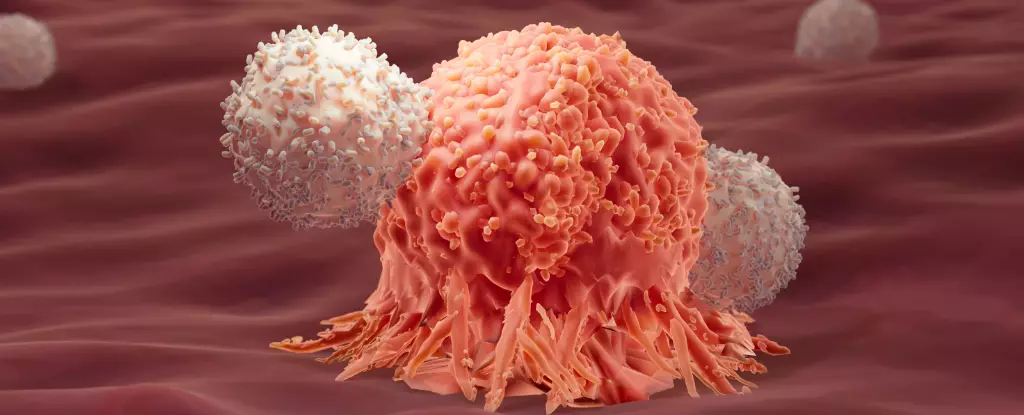
Cancer treatment has long been a landscape of scientific exploration, continually unveiling new avenues to empower the body’s defenses against the disease. Recent findings have introduced a transformative concept regarding the immune response in cancer patients. By understanding the interplay between different immune responses, researchers are now postulating that a comprehensive approach—which includes activating lesser-known immune pathways—may significantly enhance the effectiveness of cancer immunotherapy.
Immunotherapy, particularly through methods like CAR-T cell therapy, has revolutionized the treatment protocols for various cancer types. CAR-T therapy involves modifying a patient’s T cells to better recognize and attack their cancer cells, and while it has yielded remarkable results, particularly against blood cancers such as acute lymphoblastic leukemia (ALL), the journey isn’t seamless. Up to 50% of patients may experience a relapse within a year, prompting urgent research to discern the underlying mechanisms that contribute to long-term remissions.
Current insights from two pivotal studies spearheaded by researchers at École Polytechnique Fédérale de Lausanne (EPFL) reveal a profound connection between immune response types that had previously been viewed as antagonistic in nature. Specifically, while type 1 immune responses are generally seen as essential to combating cancers, it appears that type 2 responses—often associated with responses to larger pathogens like parasites—may play a crucial role in enhancing the effectiveness of immunotherapy.
The Role of Dual Immune Responses in Long-term Remission
By examining extensive genetic data from nearly 700,000 CAR-T cells derived from 82 cancer patients, researchers have uncovered a noteworthy correlation. Those who enjoyed prolonged periods of remission exhibited markers indicative of type 2 immune responses alongside the conventional type 1 responses. This unexpected association challenges prior assumptions that type 2 responses were irrelevant, or even detrimental, to combating cancer.
While correlation does not equate to causation, the implications of these findings are significant. The study prompts a reevaluation of how we classify immune responses and their roles in cancer immunotherapy.
A second study reinforced these findings, conducting experimental trials on mice afflicted with colon adenocarcinoma. Mice that received a combination of type 1 and enhanced type 2 immune responses demonstrated a striking 86% cure rate. In stark contrast, none of the mice receiving type 1 alone survived their diagnosis. This revelation showcases the potential of harnessing dual immune responses to transform typically challenging cancers, particularly solid tumors, which historically have demonstrated resistance to immunotherapy interventions.
A closer examination of the therapeutic implications revealed intriguing mechanisms at play. The modified type 2 immune proteins activated a metabolic pathway known as glycolysis, serving as an energy source for the T cells, thereby enhancing their resilience and ability to continue combating cancerous cells. This suggests that the synergy between type 1 and type 2 immune responses might function akin to the philosophical concept of “yin and yang,” where opposing forces complement each other to forge a harmonized system of defense.
As the discourse surrounding these findings continues, researchers emphasize the need for further investigation to establish whether this observed correlation can lead to definitive therapeutic strategies. The potential to implement dual-response immunotherapy could pave the way for innovative paradigms that enhance the survival rates of cancer patients, particularly those classified under challenging conditions.
Future Directions: Towards Comprehensive Cancer Treatment
The exploration of immune response synergy in treating cancer is only beginning. Should ongoing research validate these discoveries, the implications could dramatically reshape therapeutic approaches, enabling tailored treatments for individual patients based not just on the type of cancer, but also on the unique immune response profiles of each patient.
As we stand at this exciting intersection of immunology and oncology, the importance of continued inquiry and clinical trials is paramount. The aspiration for a more effective cancer treatment regime hinges on our collective ability to adapt and innovate, harnessing the full potential of the body’s immune capabilities. With promising studies like these, the future of cancer treatment appears to be on the cusp of monumental transformation—driving hope for enhanced resilience against one of humanity’s most formidable health challenges.