Ovarian cancer remains one of the most lethal malignancies affecting women worldwide, particularly in its high-grade serous form (HGSOC). The prognosis is grim, with many patients succumbing within five years of diagnosis, primarily due to late-stage detection. Current understanding, largely accumulated over a decade, points to the fallopian tubes as the potential origin of many ovarian cancers, challenging conventional views that focused exclusively on the ovaries. A recent study conducted by scientists at Cornell University, led by pathologist Alexander Nikitin, has begun to critically clarify the cellular foundations of HGSOC.
This pivotal research centers on identifying the specific cell types implicated in tumorigenesis, particularly within the oviducts of mice. As researchers investigate these cellular dynamics, an opportunity arises to significantly improve early detection and intervention strategies for this aggressive cancer. This breakthrough could not only transform patient prognoses but also advance the broader field of oncological research.
The study’s findings emerge from an experimental framework where scientists examined various cell types within the mouse oviduct. Previous studies had identified stem cells in the ovaries that could instigate HGSOC, but the research team’s focus on the oviduct marks a notable shift in the inquiry. By meticulously cataloging all cell types present in the oviduct, their work provides the first comprehensive look at the cellular landscape susceptible to ovarian cancer.
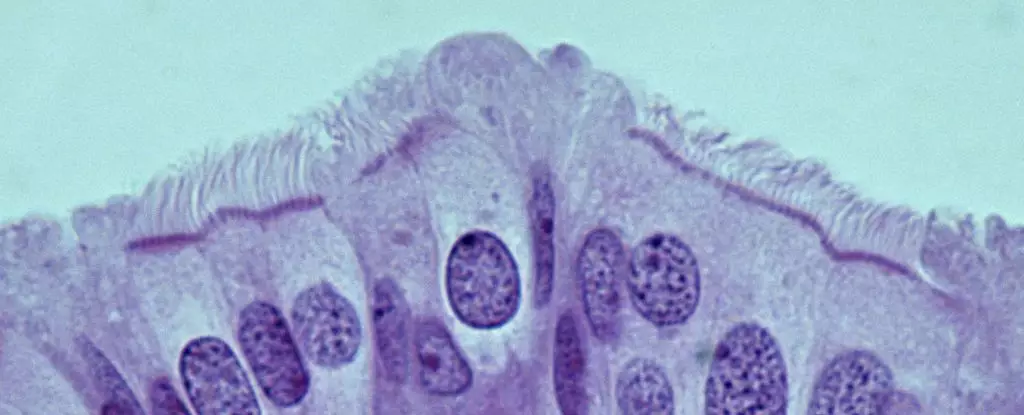
Intriguingly, the results revealed that the most cancer-prone cells in the oviduct are not stem cells, as previously hypothesized, but rather pre-ciliated cells. These cells are in a transitional phase of development, poised to become ciliated cells that play a crucial role in the transportation of oocytes. The connection between cilia formation and cancer risk is a significant finding that links normal cellular function with oncogenesis, presenting a potential avenue for further exploration.
A particularly striking aspect of this research involves the role of genetic mutations associated with HGSOC. The study indicated that two specific mutations, when present in the pre-ciliated cells, significantly enhance the likelihood of cancer formation. This relationship underscores the complexity of cancer biology, suggesting that the interplay between genetic predisposition and cellular state can give rise to malignancy.
Moreover, the implications of these findings extend beyond ovarian cancer. As highlighted by the researchers, defects in cilia formation (ciliogenesis) are also implicated in other types of cancers, notably pancreatic cancer. This suggests a broader, possibly fundamental, link in the pathways of different malignancies, emphasizing the need for interdisciplinary research approaches that can pool insights from various fields of cancer research.
The journey ahead involves a deeper investigation into the mechanisms that trigger tumor formation in these cells. Understanding the precise pathways through which genetic mutations influence pre-ciliated cells could potentially lead to the identification of novel diagnostic markers and therapeutic targets. Such advancements would be crucial for improving early detection strategies, allowing for timely interventions that could save countless lives.
The research conducted by Nikitin and his team represents a critical step forward in our understanding of ovarian cancer. As they work to transition these findings from mouse models to human applications, the potential for breakthroughs in early detection and treatment becomes palpable. The hope is that as knowledge grows, so too will the optimism for patients diagnosed with HGSOC—a disease that has long been viewed through a lens of limited hope and high mortality.
This study exemplifies the ongoing evolution of cancer research. It underscores the importance of understanding the cellular origins of disease and opens up exciting avenues for future exploration that could significantly enhance patient care and outcomes in ovarian cancer treatment. The promise of these discoveries serves as a beacon of hope for improved cancer management, highlighting the critical nexus between basic science and clinical application.