In a remarkable study showcasing the potential for revolutionary advancements in emergency medicine, scientists have demonstrated that they can revive brain activity in pigs even an hour after the cessation of circulation. Conducted by a team from Sun Yat-Sen University in China, this research presents not only a significant leap in our understanding of brain functionality post-cardiac arrest but also offers hope for extending the critical resuscitation window for human patients.
The Mechanism of Cardiac Arrest and Ischemia
The consequences of sudden cardiac arrest are catastrophic, primarily due to the abrupt cessation of blood flow throughout the body. This condition leads to ischemia, particularly detrimental when it occurs in the brain, where oxygen deprivation can result in irreversible damage within a matter of minutes. The urgency of rapid intervention aligns with the short timeframe available for effective resuscitation, hence the significance of this study. However, the research has pointed towards the liver as a pivotal player in this process—a discovery announced with anticipation by the scientific community.
Understanding the Role of Organs in Recovery
Previous studies have indicated that multi-organ ischemia influences brain recovery; however, individual organ contributions had not been thoroughly investigated prior to this study. Utilizing a model based on Tibetan minipigs, the research team set out to explore the effects of an unharmed liver on the revival of brain function following ischemic events. By studying the interactions between the liver and the brain during critical recovery phases, this research opens doors to potential medical interventions that were previously not considered.
The Experimental Framework
For the experiment, 17 lab-raised Tibetan minipigs were divided into distinct groups to assess the implications of liver involvement during brain resuscitation. Pigs in one group underwent brain ischemia for 30 minutes, while a control group experienced no ischemia, and another group was subjected to simultaneous liver ischemia. Upon examination, the results were enlightening: the control group exhibited the least brain damage, while animals that had not experienced liver ischemia demonstrated significantly lesser damage than those that had. This finding highlighted the liver’s essential role during the resuscitation process.
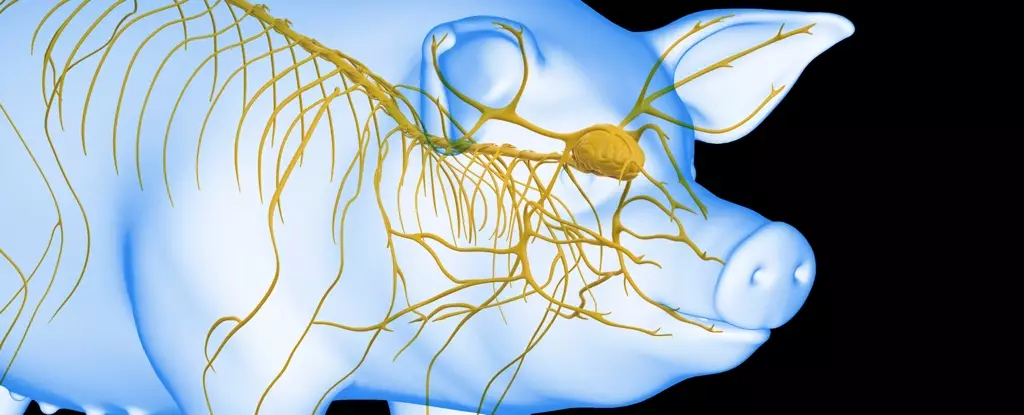
The subsequent phase of research involved a more complex intervention where an undamaged liver was integrated into an artificial life support system set to revive a brain completely disconnected from a pig body. Dubbed liver-assisted brain normothermic machine perfusion, the system connected the brain to an artificial heart and lungs to facilitate fluid circulation. The experiments varied in timing, connecting the brain to the system at intervals ranging from 10 minutes to a staggering 240 minutes post-circulation arrest.
Remarkably, the liveliness of the brains varied depending on how long they had been deprived of blood. The critical takeaway from the experiments was profound; brains connected to the system at 50 minutes post-ischemia showed sustained electrical activity for an impressive six hours. This period pointed towards critical timelines for effective revival, suggesting that there may be feasible windows for resuscitation that could save lives in emergency situations.
The implications of this research extend far beyond laboratory settings. Should these findings be replicated and understood in human models, we may witness a paradigm shift in emergency medical protocols for cardiac arrest patients. The integration of the liver’s function into resuscitation techniques could enhance recovery outcomes and survival rates significantly. Moreover, it reinforces the importance of interdisciplinary studies that examine the interconnected roles of the body’s systems in healing processes.
Furthermore, as research proceeds, it may pave the way for improved protocols in transplant medicine and critical care, taking into account the contribution of organ systems that were previously underestimated. Collaborative efforts among neurologists, cardiologists, and transplant specialists may yield new strategies for combatting the irreversible effects of ischemia.
The study led by Xiaoshun He and his team is a pioneering step towards redefining our understanding of post-cardiac arrest recoveries. The discovery of the liver’s beneficial role in brain resuscitation opens exciting pathways for future research and treatment modalities, heralding an era where medicine may conquer limitations previously thought insurmountable in critical care. Understanding these dynamics will be vital in developing new interventions that not only extend the hope of survival but also the quality of life for patients post-recovery.