Glioblastoma stands as the most prevalent and lethal variant of brain cancer, posing significant challenges to patients and healthcare professionals. The stark reality is that following a diagnosis, the average patient only lives between 12 and 15 months. Further compounding the tragedy, merely 6.9% of individuals survive beyond a five-year mark, which categorizes glioblastoma as one of the most grievously underestimated cancers in terms of survival prospects.
The impacts of glioblastoma extend far beyond mere survival statistics. Patients often endure a host of debilitating symptoms, including severe headaches, seizures, and changes in cognitive functions and personality. These neurological impairments can drastically diminish the quality of life, placing an emotional and physical burden not only on the patients but also on their families. The hope for targeted treatments has been a long-standing desire in the medical community, yet progress has been painfully limited.
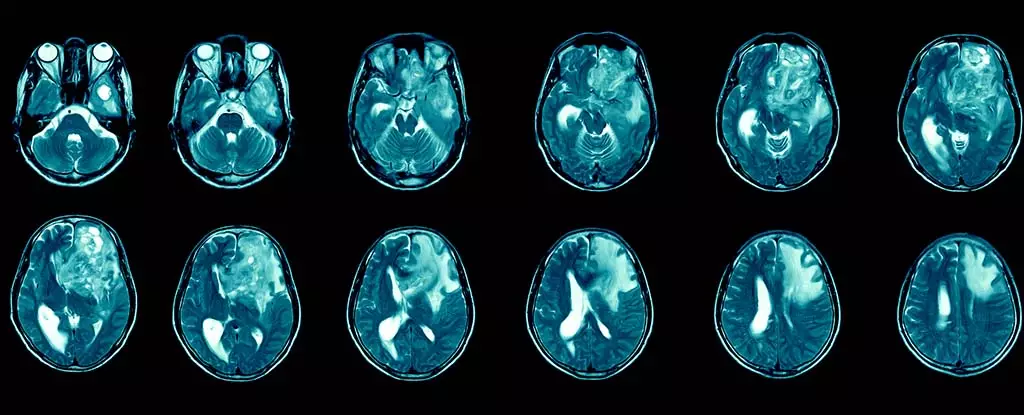
Glioblastoma belongs to a broader classification known as gliomas, which are tumors that originate from glial cells in the brain and spinal cord. Recognized as a grade 4 tumor by the World Health Organization, glioblastoma is notoriously aggressive. In the United Kingdom alone, approximately 3,200 new cases arise each year, contributing significantly to the 12,700 brain and central nervous system tumors diagnosed annually. This widespread occurrence translates into an alarming global incidence of around 3.2 to 4.2 cases per 100,000 individuals, leading to about 150,000 new patients worldwide annually.
Standard treatment protocols—including surgical intervention, radiation therapy, and chemotherapy—frequently show only transient effectiveness. The tumor’s remarkable capability to evade conventional treatments, combined with the formidable blood-brain barrier that limits drug delivery, enhances the complexity of managing this disease. Unfortunately, even after surgery, the likelihood of tumor recurrence remains high, leading to additional challenges in treatment and long-term management.
Recent advancements in immunotherapy offer a potentially transformative approach, harnessing the body’s immune system to target and destroy cancer cells. The therapeutic landscape for other cancers, such as melanoma and lung cancer, highlights the promise of immunotherapy, but glioblastoma presents unique hurdles. Its evolutionarily dynamic nature results in diverse mutations across different brain regions, complicating treatment efforts.
Encouraging research indicates that immunotherapy may be administrated via injections into the cerebrospinal fluid—a method showing promise for improved drug delivery. Ongoing studies aspire to refine these techniques, aiming to enhance penetration of the tumor while minimizing damage to surrounding healthy tissue. However, the road to effective immunotherapy for glioblastoma remains fraught with challenges, including variability in individual responses and potential immune-related side effects such as organ inflammation.
Historically, funding limitations have posed significant barriers to glioblastoma research. Nonetheless, emerging initiatives are striving to attract researchers from diverse scientific backgrounds to address this grave issue. The collaborative effort extends to experts like myself, who have dedicated decades to understanding immune modulation during cancer and chronic infections. Recently, I have turned my focus toward brain function and its relationship with immune responses, merging this knowledge with glioblastoma research.
As part of a larger mission, my ongoing investigations aim to identify strategies to penetrate barriers that prevent treatments from reaching tumors. This work exemplifies the necessary interdisciplinary approach to tackle the complexities inherent in glioblastoma.
While comprehensive immunotherapies for glioblastoma remain nonexistent, the landscape of research is evolving, suggesting a potential turning point for more effective therapeutic options. It is critical to note that immunotherapy does not yield favorable results for every cancer type, and careful management of any potential side effects, particularly those affecting the brain, is essential.
In reevaluating treatment delivery methods, researchers are prioritizing less invasive options, favoring approaches such as spinal injections over traditional surgical interventions. This evolution of methodology is crucial for yielding better outcomes and minimizing patient discomfort.
The hope surrounding immunotherapy for glioblastoma is palpable and backed by growing interest and funding. As ongoing studies unfold, the aspiration for breakthroughs becomes more attainable. Continued collaboration, investment, and dedication to understanding the nuanced nature of glioblastoma could herald a new era in treatment, offering renewed hope to patients and their families facing the harsh realities of this formidable disease.