Recently, the U.S. has witnessed a concerning development in public health as an elderly patient in Louisiana has been reported in “critical condition” due to the avian influenza, specifically the H5N1 strain. This case marks a significant escalation in the ongoing avian influenza outbreak, indicating that there’s more at stake than initial mild symptoms exhibited by other patients. Up to this point, the total number of infections in the United States during the 2024 avian flu outbreak has reached 61, raising alarms across the nation, particularly as California has declared a state of emergency to bolster its response efforts.
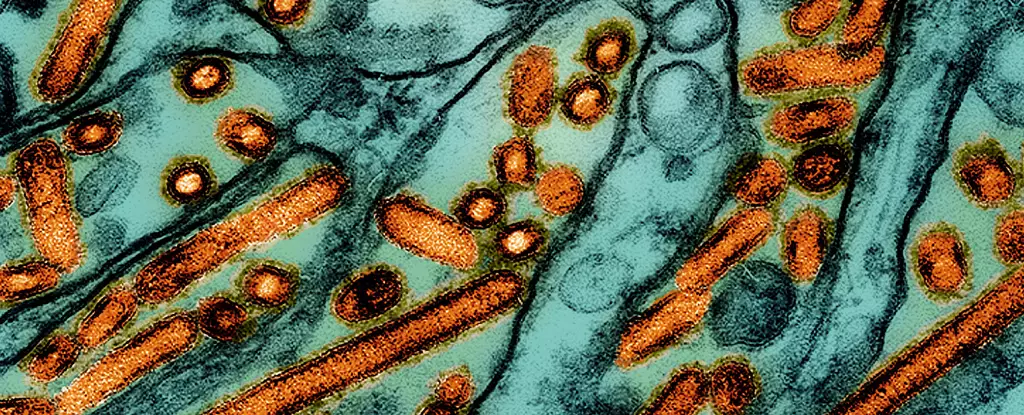
The implications of this singular, severe case amplify fears regarding a potential bird flu pandemic. With prior infections mostly resulting in symptoms that were manageable at home, the Louisiana case starkly contrasts with the image painted by past experiences and suggests that the H5N1 virus’s capacity for human infection may be more serious than previously anticipated.
According to the Centers for Disease Control and Prevention (CDC), this Louisiana patient was likely exposed to the virus by interacting with sick and deceased birds in backyard flocks. The severity of the illness—characterized by significant respiratory distress—raises critical questions about the routes of transmission, particularly in light of the known presence of the virus in wildlife and poultry.
Health officials have indicated that H5N1 has a documented history of causing severe illness globally, with mortality rates reaching alarming heights of up to 50% in documented cases. As CDC senior official Demetre Daskalakis pointed out, the established severity associated with this virus underlines the necessity of a comprehensive federal response—a call to action that cannot be taken lightly, especially considering the severity of the current case.
The state of emergency declared in California highlights the urgency for local and federal authorities to take proactive measures. California Governor Gavin Newsom emphasized that this proclamation serves as a critical mechanism to ensure that resources are mobilized swiftly, allowing government agencies to effectively monitor and preemptively tackle the outbreak. This proactive approach illustrates a heightened state of alert, given that the virus’s most recent genotype, D1.1, has been detected in various regions, linking it to cases not only within the United States but also in neighboring Canada.
Genetic analysis shows that this new strain shares characteristics distinct from other known strains, adding complexity to the public health landscape. The emergence of a strain that can spread among wildlife and potentially infect humans underscores the importance of surveillance, coordination, and preparedness in mitigating the risk of a more widespread outbreak.
The current situation has ignited discourse among scientists and health experts about the adequacy of surveillance in capturing the entire scope of animal-to-human spillovers. Rebecca Christofferson from Louisiana State University has aptly noted that insufficient surveillance may obscure the extent of potential human infections, particularly those occurring without obvious animal vectors. While some experts remain cautiously optimistic, emphasizing that there is no immediate reason to panic, they also stress the need for heightened vigilance.
In stark contrast, epidemiologist Meg Schaeffer of SAS Institute has pointed out several factors that bolster the case for concern, insisting that avian flu could potentially catalyze a new pandemic if not monitored closely. This duality in perspective illustrates the need for a balanced approach—to remain alert to the real risks posed by emerging infectious diseases while also fostering public understanding and preparedness.
With the threat of avian influenza looming, the U.S. has taken preventative strides by stockpiling vaccines for bird flu. Recent studies have revealed promising results for experimental mRNA vaccines, which have shown effectiveness in protecting ferrets against the virus. This push for vaccination emphasizes a broader strategy aimed at not only protecting poultry but also safeguarding public health from potential human transmission.
Moreover, regulatory measures are tightening, as indicated by the U.S. Department of Agriculture’s mandate related to raw milk testing protocols. By enforcing stringent reporting requirements for any detected avian flu in dairy products, authorities are attempting to close any gaps in transmission pathways that could potentially endanger public health.
The resurgence of avian influenza, particularly in light of alarming cases like that in Louisiana, serves as a sobering reminder of the interconnectedness of animal and human health. As health officials, scientists, and policymakers navigate this evolving landscape, it is essential to foster a climate of preparedness and awareness. Through enhanced surveillance, increased public education, and a commitment to research and vaccine development, the threat of avian flu can be managed, ensuring that history does not repeat itself in the form of a pandemic.