The intricate and often underestimated relationship between hormones and the brain is a vital area of study, especially in the context of the menstrual cycle. Traditionally, discussions surrounding menstruation have focused on its physical effects or the emotional upheaval it may cause. However, emerging research shines a spotlight on how menstrual hormones not only impact reproductive health but also profoundly influence brain structure and function. A recent study led by researchers from the University of California Santa Barbara underscores this paradigm shift, illustrating that the effects of menstruation extend far beyond physical sensations and mood swings.
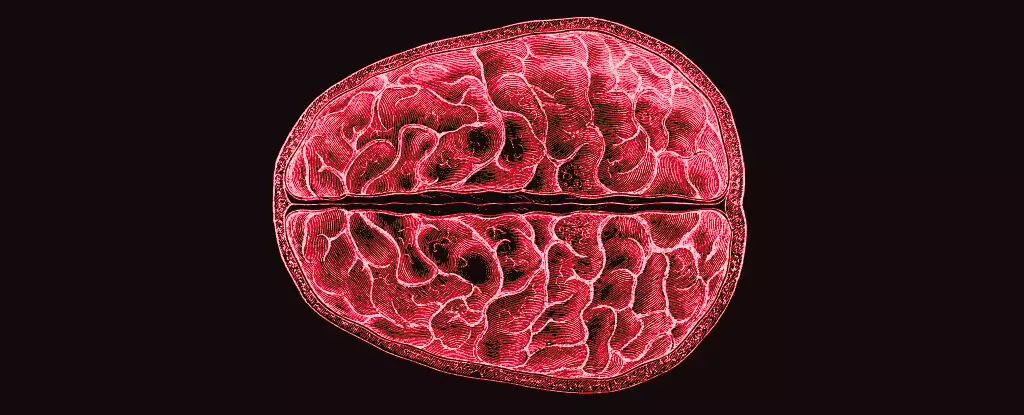
The research team, comprised of neuroscientists including Elizabeth Rizor and Viktoriya Babenko, meticulously tracked variations in brain structure across different phases of the menstrual cycle among 30 women. Their findings, which were published in a peer-reviewed journal in 2023, fundamentally challenge our understanding of hormonal effects on the brain. The study reveals simultaneous changes in white matter microstructure and cortical thickness correlated with hormonal fluctuations. Such insights are groundbreaking; they highlight that the impact of menstrual hormones is not confined to traditional centers of reproductive function in the brain, but rather encompasses a broader range of brain regions.
Bridging the Gap in Research
Despite the fact that menstruation affects almost half the world’s population for a significant portion of their lives, there remains a puzzling lack of research focusing on its cognitive and neurological implications. This oversight raises critical questions about societal attitudes towards women’s health and reproductive rights. Why is there such ambiguity surrounding a phenomenon that is both universal and profound? The answer may lie in a historical underappreciation of women’s health issues in scientific research, leading to gaps in knowledge that extend to important aspects of brain function and mental health.
Rizor and her team pointed out that while cyclical fluctuations in hormones have documented effects on behavior, much less is understood about how these changes impact the fundamental structure of the brain. Existing studies have primarily explored brain communication during cognitive tasks but have overlooked the physical transformations occurring during the menstrual cycle. Recognizing the brain as a dynamic entity that adapts continuously in response to hormonal changes accentuates the need for further interdisciplinary research that amalgamates neuroscience, psychology, and gynecology.
Hormonal Changes and Their Psychological Impact
The team’s striking findings suggest that hormonal shifts significantly influence the brain’s white and gray matter. For instance, the research notes that increased levels of estradiol and luteinizing hormone prior to ovulation are linked with changes in white matter that can enhance the speed of information transfer. These findings indicate a potential cognitive edge during specific phases of the menstrual cycle, which could explain variations in mood, focus, and emotional resilience experienced by many women.
Furthermore, as progesterone surges after ovulation, there is a corresponding increase in tissue density and a reduction in cerebrospinal fluid volume. This complex dance of hormones and brain structure raises intriguing possibilities for understanding the roots of certain mental health challenges faced during menstruation. Disorders such as premenstrual syndrome (PMS) or premenstrual dysphoric disorder (PMDD) may have biological underpinnings related to these structural changes, opening the door to potential interventions that target hormonal pathways.
Rethinking Women’s Health Research
Ultimately, the findings from this research serve as a compelling call to action for the scientific community. Understanding how hormonal cycles influence brain structure is essential not just for recognizing normal variations in mental health but also for addressing severe menstrual-related conditions that can undermined quality of life. By prioritizing research into the brain’s response to menstrual hormones, we can foster a more nuanced understanding of women’s health that goes beyond mere anecdotal evidence.
There is an urgent need to advance how we study and discuss woman-centric health issues, ensuring that they are placed at the forefront of neuroscience. This shift will not only empower women with knowledge about their bodies and brains but also prompt medical practitioners to adopt more holistic approaches to treatment. Just as our understanding of the menstrual cycle evolves, so too must our commitment to bettering women’s health through scientific inquiry.