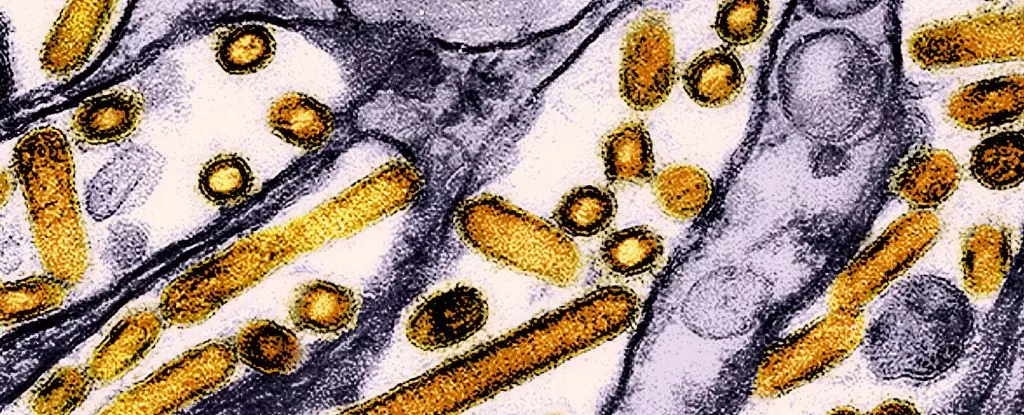
Recent investigations into the health of dairy workers across Michigan and Colorado have uncovered concerning evidence of previously undetected human infections by the highly pathogenic avian influenza virus, H5N1. Blood tests conducted by researchers from the U.S. Centers for Disease Control and Prevention (CDC) indicated that approximately 7% of the 115 dairy workers tested between June and August 2024 exhibited antibodies linked to H5N1. This revelation raises vital questions about the interaction between humans and avian viruses, particularly within agricultural settings.
Given the scale of poultry outbreaks and the extensive culling of infected birds in recent years, the detection of antibodies suggests that while many infections may have been asymptomatic or mildly symptomatic, the potential for transmission and mutation of the virus remains a significant public health concern. The majority of dairy workers with these antibodies did not report severe illness, but this scenario does not lessen the inherent risks associated with unmonitored viral evolution.
The Mutation Dilemma
Researchers are notably concerned about the possibility that allowing H5N1 to circulate without stringent control measures could lead to dangerous mutations. A recent outbreak in Cambodia serves as a stark illustration of this risk, where the emergence of a new hybrid strain demonstrated enhanced capacity for mammalian infection and airborne transmission. At least three fatalities have been reported in this case, and genetic analyses reveal mutations that facilitate this transmission. Fortunately, human-to-human transmission has not yet been observed, but as history shows, viruses can evolve rapidly and unpredictably.
The case reported in Canada, where a teenager is currently in critical condition due to a mutated version of H5N1, highlights the urgent necessity for vigilant monitoring and control strategies. Similar to the Cambodian outbreak, the genetic changes detected imply an increased ability for the virus to infect humans. Although this event appears isolated, it serves as a cautionary tale regarding the potential for sporadic cases to catalyze larger outbreaks.
The demographic of the affected dairy workers is particularly noteworthy. Most were engaged in direct contact with potentially infected animals during milking or parlor cleaning tasks. Alarmingly, none of these individuals reported using appropriate personal protective equipment (PPE) as recommended by health officials, a situation echoed across the broader agricultural community. This lack of precaution underscores a significant gap in awareness and training regarding zoonotic infections in farm environments.
Reports from the affected workers detailed symptoms such as red and itchy eyes, fever, sore throat, and other flu-like manifestations. The apparent mildness of their conditions raises questions about the overall preparedness and health education among agricultural workers, particularly those who may not be fluent in English. It is essential for health authorities to enhance outreach and training programs aimed at fostering a culture of safety and vigilance around potential zoonotic threats.
Public Health Implications
Despite the current perception of low transmission risk, the CDC and other health bodies are urging for heightened awareness and proactive measures among agricultural workers. With over 400 dairy herds infected across the United States, there is a pressing need for robust monitoring and outreach initiatives to prevent further transmission among both animal and human populations.
Effective communication strategies that are culturally sensitive are crucial, particularly for communities with high numbers of Spanish-speaking workers. The CDC plans to bolster its public health campaigns, focusing on educating employees about infection risks and promoting stringent use of PPE.
Globally, authorities are advocating for rigorous hygiene practices when coming into contact with animals, including reporting signs of sickness among birds. The consequences of allowing avian influenza to go unchecked can be devastating, with over 90 million domestic birds culled in the U.S. alone since 2022. While efforts such as vaccinations for critically endangered species like the California condor are underway, a focused global effort to develop a human vaccine is also needed.
The prospect of a mutating avian influenza virus poses a potential threat not only to agricultural workers but also to public health at large. Investments in research, education, and preventive health strategies must remain a priority to mitigate these emerging risks effectively.
The findings from Michigan and Colorado serve as an urgent call to action for both public health practitioners and agricultural workers, reminding us that diligence in monitoring, education, and protective measures is essential in the battle against zoonotic diseases.