Understanding the menstrual cycle has long been a topic of interest, not only for those who menstruate but also for the scientific community. Recent findings from a study conducted by Elizabeth Rizor and Viktoriya Babenko at the University of California, Santa Barbara, shed light on an often-overlooked aspect: the interplay between hormonal fluctuations and brain structure. Over the course of their research, they examined 30 menstruating individuals, seeking to unravel the complexities of how our hormonal profiles reverberate within the neural architecture of the brain.
Unlike conventional studies that primarily explore the cognitive dimensions of hormonal changes, this research dives deeper, offering a platform for understanding how menstrual hormones might reshape the very fabric of brain structure. The findings indicate that not only does the brain communicate differently in response to hormonal shifts, but it undergoes structural transformations as well. Such revelations challenge the simplistic view of hormones’ roles, emphasizing a more intricate dance between endocrine processes and neuroanatomy.
The impact of menstruation on mental and physical health is well-documented; however, there is a surprising scarcity of research focused on the neurological effects of menstruation itself. Women generally experience around 450 menstrual cycles over their lifetimes, yet the implications of these cycles for brain function and structure remain largely enigmatic. The ongoing gap in knowledge can be seen as a paradox in a world that prides itself on scientific advancements. Given that nearly half of the world’s population menstruates, an exploration of this area is long overdue.
The research team’s methodology incorporated MRI scanning during distinct phases of the menstrual cycle—menses, ovulation, and mid-luteal phases—allowing for a detailed assessment of structural changes in relation to hormonal surges. This approach provided an innovative perspective, capturing real-time changes and heralding a new era in the understanding of brain dynamics driven by hormonal cycles.
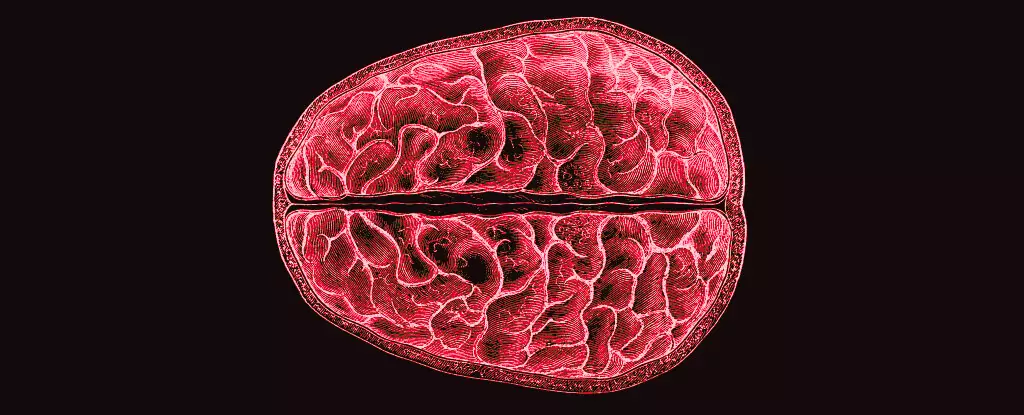
The study revealed a significant association between hormonal fluctuations and alterations in both white and gray matter, prompting questions about the implications these changes might have for cognition, behavior, and overall mental health. White matter, comprising neuron fibers enveloped in a fatty sheath, serves as an essential conduit for information within the brain. The shifts observed in this fatty network during key hormonal phases suggest not only a reorganization of cognitive pathways but potentially an increase in the brain’s efficiency in processing information.
Interestingly, the study indicated specific hormonal relationships with brain structure: The surge of hormones like 17β-estradiol and luteinizing hormone preceding ovulation correlated with enhanced white matter properties, implying faster information transfer. In contrast, progesterone’s rise after ovulation appeared to influence tissue volumes and cerebrospinal fluid dynamics. Such revelations enrich our understanding of the cyclical nature of brain function and invite further inquiry into how these structural modulations impact day-to-day mental experiences.
These findings represent an important stepping stone in bridging the menstruation gap in neuroscientific research. By highlighting the correlation between hormonal fluctuations and brain structure, they open the door to more expansive studies that could unravel the mystery surrounding menstrual-related mental health challenges. Issues such as premenstrual dysphoric disorder (PMDD) and other mood disorders may find deeper explanations in the interplay between hormones and structural brain changes.
While this study certainly provides a framework for future explorations, it also accentuates the need for a broader and more inclusive approach to research in areas traditionally dominated by male-centric studies. Expanding our understanding of menstrual health and its relationship to neuroscience could not only improve mental health care but also enrich our knowledge of human biology as a whole.
Rizor and Babenko’s research marks a significant advancement in our understanding of the monthly hormonal cycles and their comprehensive impact on brain structure. As we continue to unravel this complex relationship, the potential benefits for mental health care and personal well-being are immense. Embracing this newfound knowledge might empower both researchers and individuals who experience these cycles, fostering a greater appreciation for the biological marvels of the human body.